CMS data shows strong - but uneven - ASC growth for colorectal procedures
November 17, 2025
Colorectal problems are more common in the United States than most people realize. However, two trends may help increase early detection and treatment of these conditions. First, more adults are aware of the benefits of early screening. And at the same time, a majority of patients now prefer the comfort and convenience of ambulatory surgery centers instead of hospital outpatient departments. We analyzed CMS data in our proprietary model to learn if procedures linked to colorectal health are becoming more common in ASCs.
Colorectal disease is a major concern in the United States, with colorectal cancer the second-leading cause of cancer death. Although survival rates approach 90% when caught early, once this cancer spreads, survival drops to about 16%.
Chronic conditions such as inflammatory bowel disease (IBD) and diverticulitis also put patients at risk. People often think of these as manageable quality-of-life issues, but without timely intervention, they can progress to serious complications.
Social stigma, lack of awareness about who is at risk, and confusion about when to seek care all contribute to patients delaying or avoiding evaluation. But colorectal problems are more common in the United States than most people realize:
- IBD affects around 3 million people in the U.S.
- Diverticulitis is responsible for 300,000 hospitalizations per year and is the 4th-leading cause of emergency surgery for older adults
- 1 in 24 Americans will be diagnosed with colorectal cancer in their lifetime, with a consistent 2% annual increase among adults age 20-39 since the 1990s
However, two trends may help increase early detection and treatment of these conditions. First, more adults are aware of the benefits of early screening. And at the same time, a majority of patients now prefer the comfort and convenience of ambulatory surgery centers instead of hospital outpatient departments.
As patient preferences shift, ASCs may have an important role in expanding access to early detection and treatment. We examined our proprietary model to learn if procedures linked to colorectal health are becoming more common in ASCs. This model is derived from 100% of Centers for Medicare and Medicaid Services (CMS) data, as well as open- and closed-claim sources, covering more than 330 million patients.
For this study, we examined endoscopic (CPT codes 45300 - 45393) and laparoscopic (CPT codes 45395 - 45499) colorectal procedures as defined by the American Academy of Professional Coders (AAPC). Some procedures in this analysis include proctosigmoidoscopy, flexible colonoscopy with band ligation, laparoscopic removal of the rectum (with and without pouch), and laparoscopic colonoscopy with ablation.
ASC volume for these procedures is growing, but this trend is not uniform across the United States, raising questions of equal access to preventative care and early treatment.
Examining the northeast, south, midwest, and west as distinct regions, we find that:
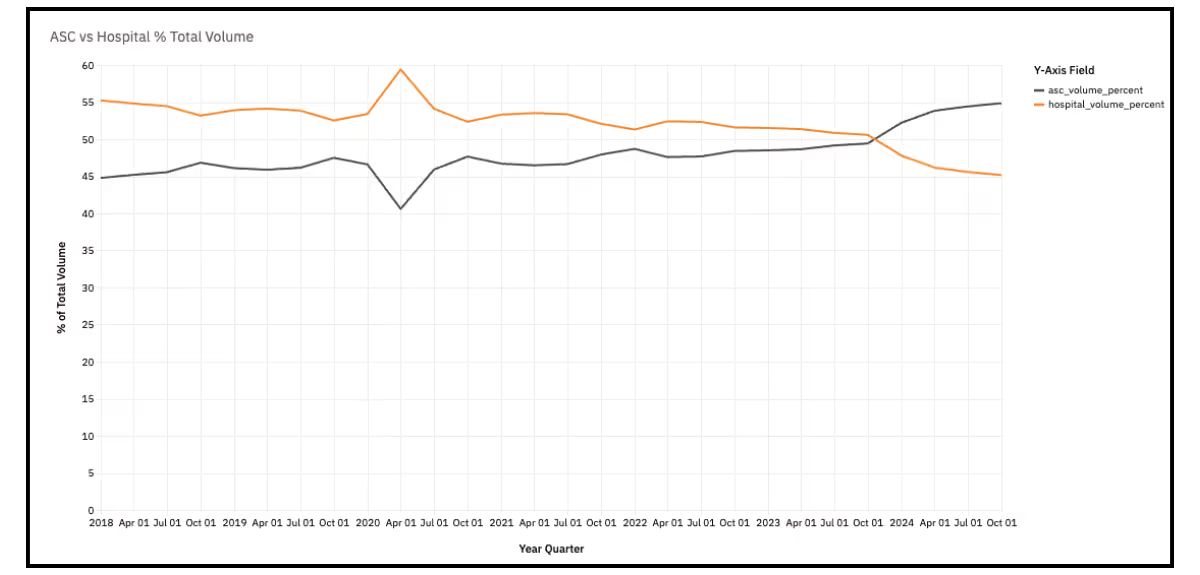
Northeast
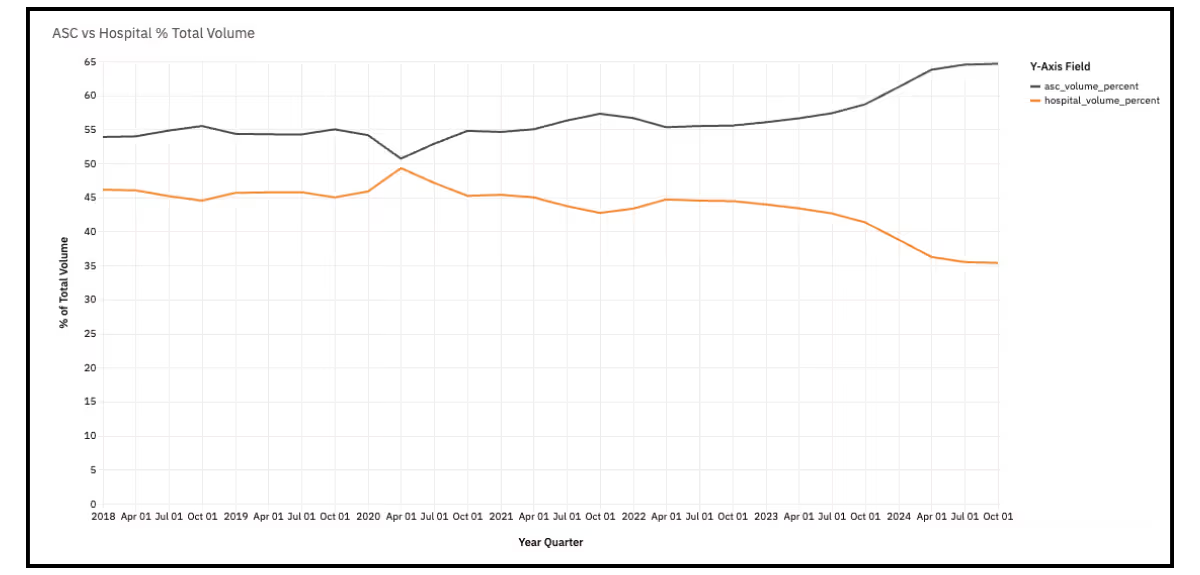
- Endoscopic volume at ASCs surpassed hospitals between Q4 2023 and Q1 2024. Now 55% of procedures occur in an ASC in the northeast.
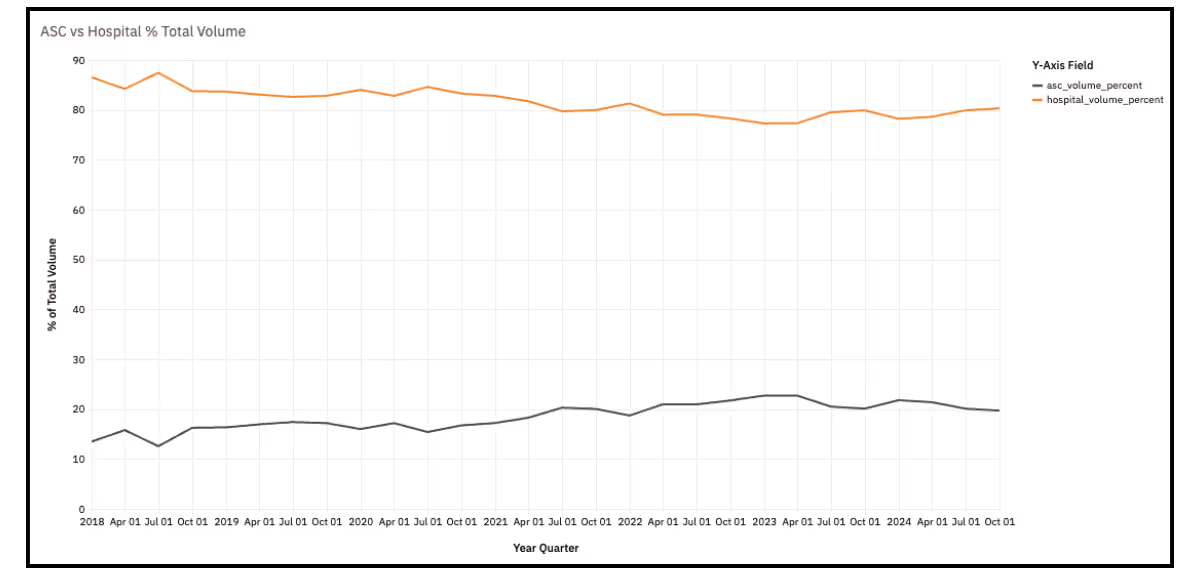
- Hospitals continue to dominate laparoscopic procedures with over 80% of volume as of Q3 2024.
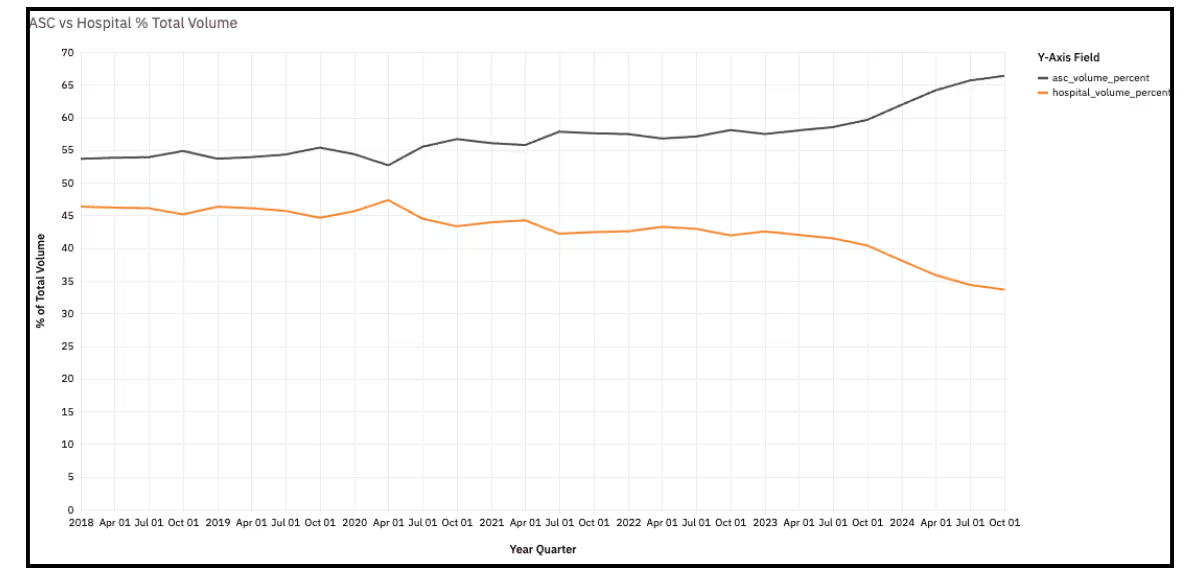
South
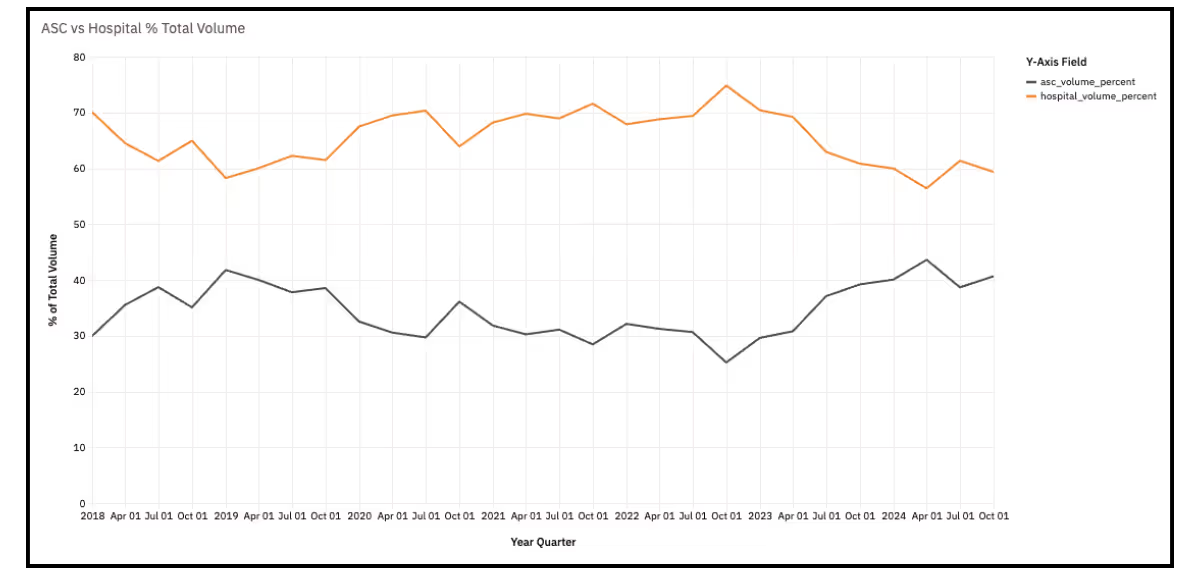
- ASCs have had a majority share of endoscopic procedures since 2018, and that share grew starting in 2023. ASCs now perform nearly 70% of endoscopic procedures in the south.
- Hospitals have a large majority of laparoscopic procedures in the south, but the ASC share has grown from under 20% in 2018 to over 30% in 2024.
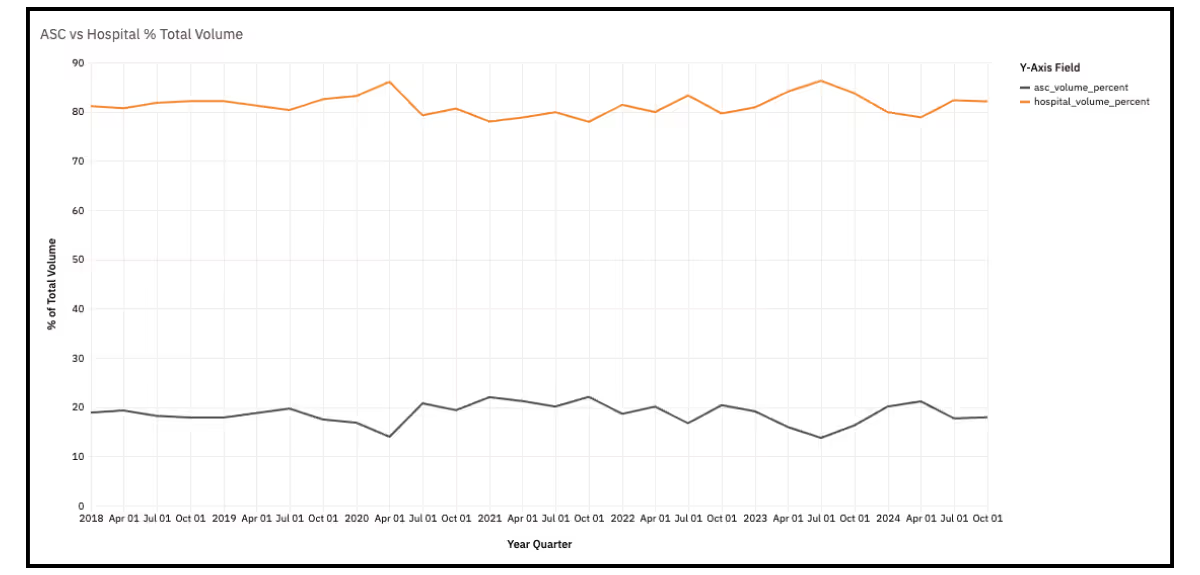
Midwest
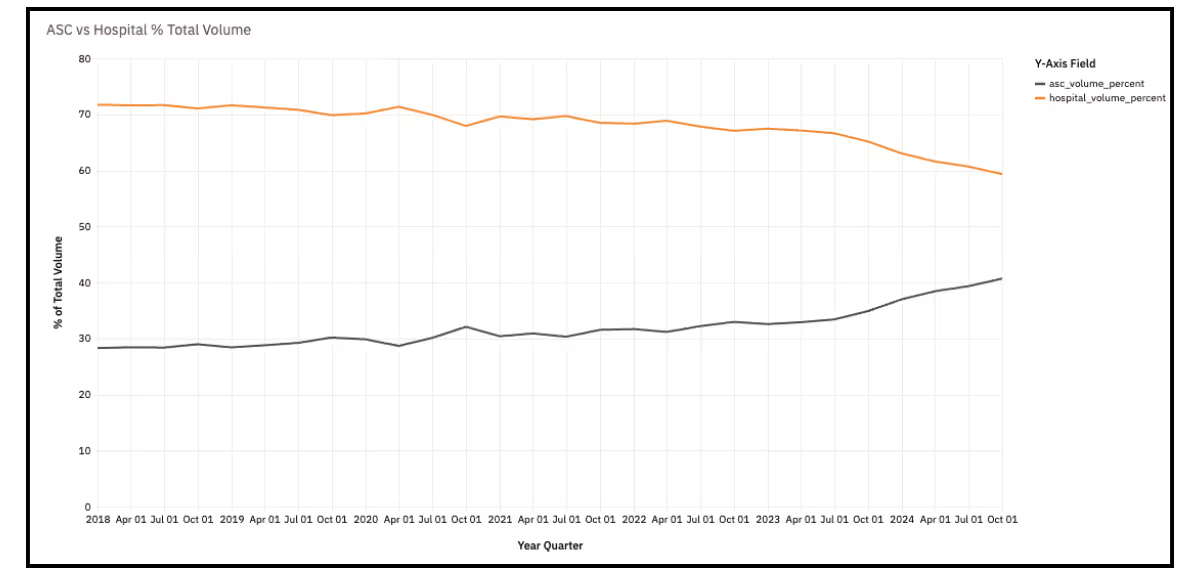
- The hospital share of endoscopic volume held around 70% from 2018 to 2023, when hospital volume began to decline and ASC volume began to increase. Although the majority of these endoscopic procedures are still done in hospitals, it’s now closer to a 60/40 split.
- Hospital laparoscopic procedures dipped in 2022 and 2023 but began to increase their share again in 2024. ASC volume is down to around 20% of total volume.
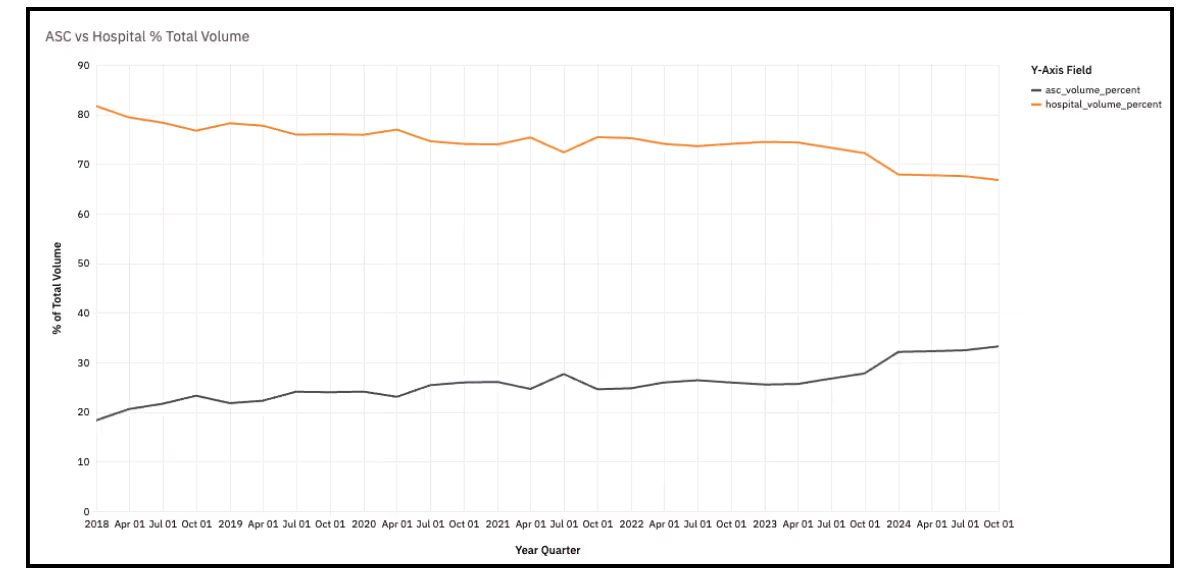
West
- Similar to the south, a majority of endoscopic procedures have been performed in an ASC since 2018. There was another sharp increase beginning Q4 2023 and ASCs now perform 65% of these procedures.
- Although hospitals still perform the majority of laparoscopic procedures, this region has seen the most fluctuation quarter to quarter, from a high of 75% in Q4 2022 to a low of 56% in Q2 2024. ASC began to gain share once again starting in Q3 2024.
Taken together, the data show that more colorectal procedures are shifting into ASCs, especially for endoscopic exams that play a central role in screening, surveillance, and early intervention. This can lower barriers to care for patients who might delay or avoid screening.
However, progress is uneven. Laparoscopic procedures - often used for more advanced disease or surgical intervention - still occur predominantly in hospitals, and both endoscopic and laparoscopic volumes vary widely by region and state. In some areas, patients may face greater obstacles to timely treatment.
The stakes are high. Routine screening and earlier treatment of abnormal findings can dramatically change outcomes for colorectal cancer, IBD, and diverticular disease. The trends in this analysis are encouraging because they suggest growing options for where patients can receive care. But the regional gaps also highlight an important public health priority: continuing to increase awareness of the importance of colorectal screening and care while incentivizing increased access to those procedures so more patients can benefit from early detection and prompt treatment.