Come see us at Flywheel 2025! Register Now »
Hospitals and health systems have been under financial strain for years due to increasing costs and shrinking reimbursements, but 2025 has brought new urgency. With increased tariffs and looming cuts to Medicare and Medicaid, many healthcare executives are revising their long-term strategies. Financial sustainability is no longer a background concern; it’s the primary lens through which many decisions are made.
As Mary N. Mannix, president and CEO of Augusta Health in Fisherville, VA recently explained to Becker's Hospital Review, “We need to be clear on the materiality of these cuts and the tangential consequences, such as losing eligibility to participate in the 340B program.” Mannix added that Augusta Health was now trying to match their existing five-year plan to new economic realities.
Doug Watson, executive vice president and CFO of Allina Health in Minneapolis, MN is also concerned with the cuts coming to Medicare in two years, noting the combination of increased costs and these cuts will mean that “The ability to maintain current healthcare services and infrastructure in our area will be seriously challenged with drastic cuts to Medicaid.”
For MedTech companies, this mindset shift changes the game. It will be very difficult to convince a value analysis committee (VAC) to replace existing products with more expensive options, or to adopt new technology based mainly on clinical comparisons. To succeed, MedTech commercial teams must leverage market intelligence and accurate healthcare data to prove how their technology either increases revenue, helps prevent patient leakage, or reduces costs.
AcuityMD has the precise market data and simple workflows to help MedTech commercial teams create a GTM playbook centered on ROI that's tailored to the challenges hospitals and health systems are facing.
With reimbursement cuts looming, reps can’t afford to spend time targeting sites where payer mix makes ROI difficult. AcuityMD Payer Mix gives MedTech reps details on how payers reimburse certain procedures - and at what rate - at a facility. With these insights, reps can build a pitch that addresses growing financial challenges. If a payer offers better reimbursement for your device, it could incentivize a site of care to switch to your product. On the other hand, if a facility heavily relies on Medicare and CMS doesn’t provide strong reimbursement for your product, a rep can deprioritize this target because of the small chance of success.

VACs don’t just consider cost when making purchasing decisions. Value in a medical device can also come from improved patient outcomes or the ability to treat more patients. AcuityMD Care Journeys uses longitudinal patient data to connect diagnoses and treatments across providers and sites of care. With this impactful visualization, MedTech reps can quickly demonstrate how their technology clearly improves outcomes compared to a site of care’s existing treatment options.
This can help drive ROI in multiple ways. Reps can detail how a site of care could reduce unexpected costs incurred from readmission penalties, for example. Care Journeys also lets healthcare executives see how many patients with a certain diagnosis are in their region so they understand their total available market. If another site of care 30 miles away is treating more patients because they offer your new technology and the site you’re visiting doesn’t, that’s another way for a rep to build a strong ROI case.
Additionally, reps can use Referral Pathways to show healthcare executives how they can help drive ROI by reducing patient leakage. With the ability to visualize upstream and downstream referrals between providers, healthcare executives can see where patients are leaving their systems. Providers who don’t meet benchmarks for in-network referrals can be prioritized for educational events about the benefits of your technology.

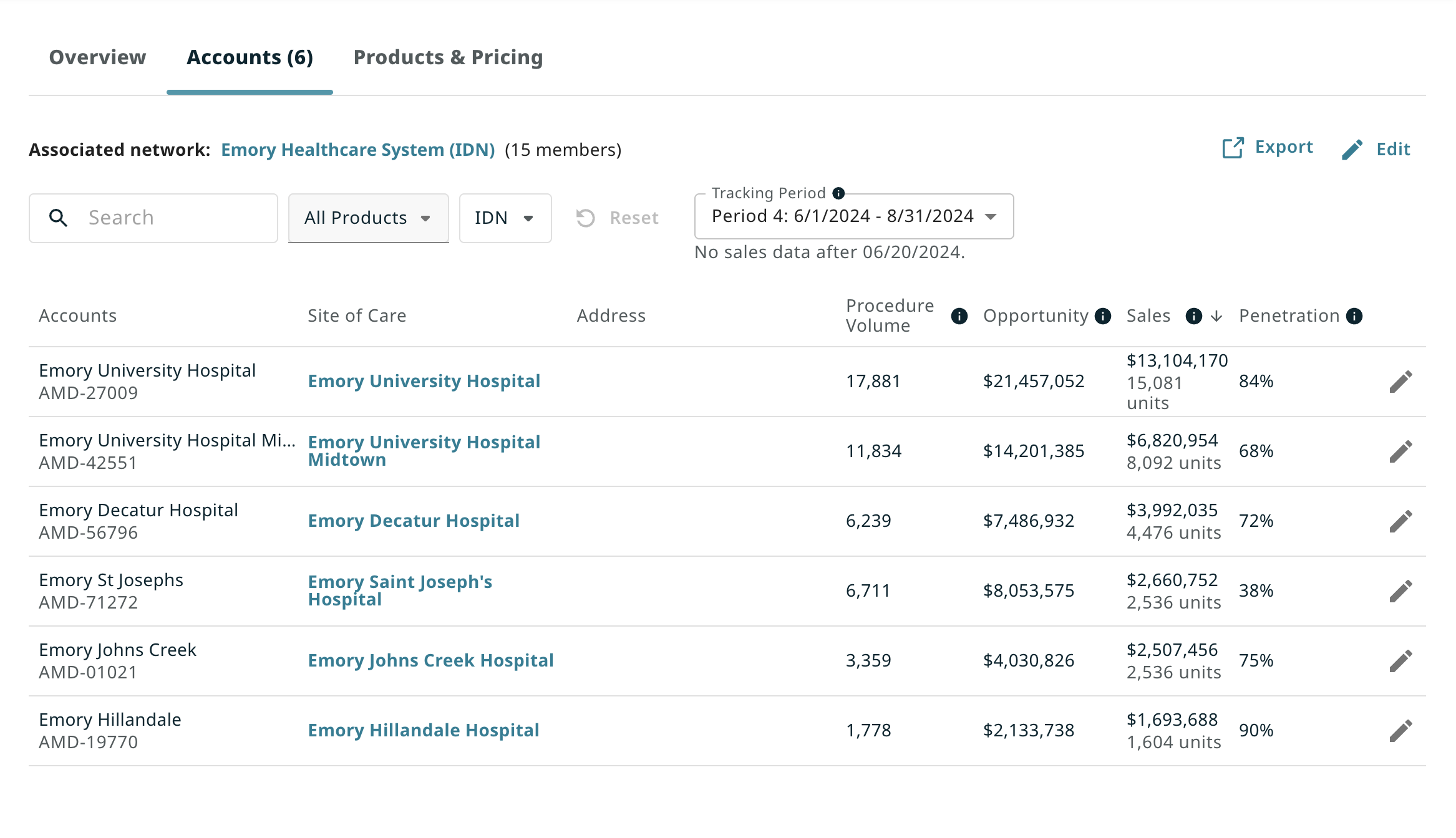
Laying contract details over procedure data uncovers whitespace and easy growth potential, and helps a rep maximize the value of their existing contracts. By referencing AcuityMD Contracts, a rep could see that one of their site of care customers needs to increase product usage to trigger volume discounts, and flag this as another route to reducing costs and improving ROI. MedTech commercial leaders can also use this data to build strategic portfolio packages that can be used to cross-sell at on-contract facilities.
The financial concerns hospitals and health systems are trying to address will be an issue for the next few years at minimum. As Lisa Goodlett, senior vice president, CFO and treasurer of Duke University Health System in Durham, N.C. stated, “We recognize that we are at a pivotal moment: To ensure long-term sustainability and value, we are taking bold, deliberate steps to enhance operational efficiency and build a more cost-effective operational structure.”
With the precise insights and intuitive workflows in AcuityMD, MedTech commercial teams can go well beyond simple discounts and price cuts to strategically position themselves as market leaders and consultative partners completely in tune with current challenges. The companies that continue leaning into traditional strategies based on relationships and gut instinct risk wasting time on targets that aren’t a match and hearing “no” more often. Those that arm their reps with financial insights, and the tools to translate them into compelling ROI stories, will be the ones that win more often.